Latest update, November 15, 2021: This blog post has lots more information on what I’ve learned and what I’m doing about it. The FitEyes community makes clear, once again, that when e-patients get to research their condition and talk to each other, far more information flows than what happens in a typical doctor visit. It’s good!
Update November 9: I’m going to stop updating this page because I’ve found exactly the kind of savvy, street-wise patient community I’ve wanted! FitEyes.com, with its companion sites discuss.fiteyes.com (an email group) and a new resource site they’re developing called Ask.FitEyes.com.
See you there – I hope to help further develop what they do into increasingly useful resources for people who are new to glaucoma!
Original text of this page – unfinished notes I gathered early on
Last updated 6/25/21 with new section at bottom on the problems of preservatives in eye drops.
This is not medical advice; it’s my own collection of notes. I’m not a medical authority. You’re welcome to read, but you’re responsible for any decisions you make. I always urge everyone to verify on their own before taking any action, as I always do.
Comments and questions are welcome at bottom of page.
In February 2021 I was diagnosed with glaucoma in my left eye. Glaucoma produces irreversible damage – it’s rather like an amputation (a permanent loss) except you can’t get a replacement “limb.” (Yet.) I’ll use this page as my “outboard memory,” as Susannah Fox puts it – a place to store things so I know where to find them.
Introduction to glaucoma
I’ve been surprised how hard it was to get a good clear introduction to what the disease is. Example: one site said it’s “an increase in intraocular pressure that causes pathologic changes in the optic disk and typical defects in the field of vision.” Huh?? That may be fine for scientists describing things to each other, but it’s useless to a newly diagnosed patient.
Please, experts: empower and inform us, don’t confuse us! We need to know what’s going on in this body, and what can be done about it.
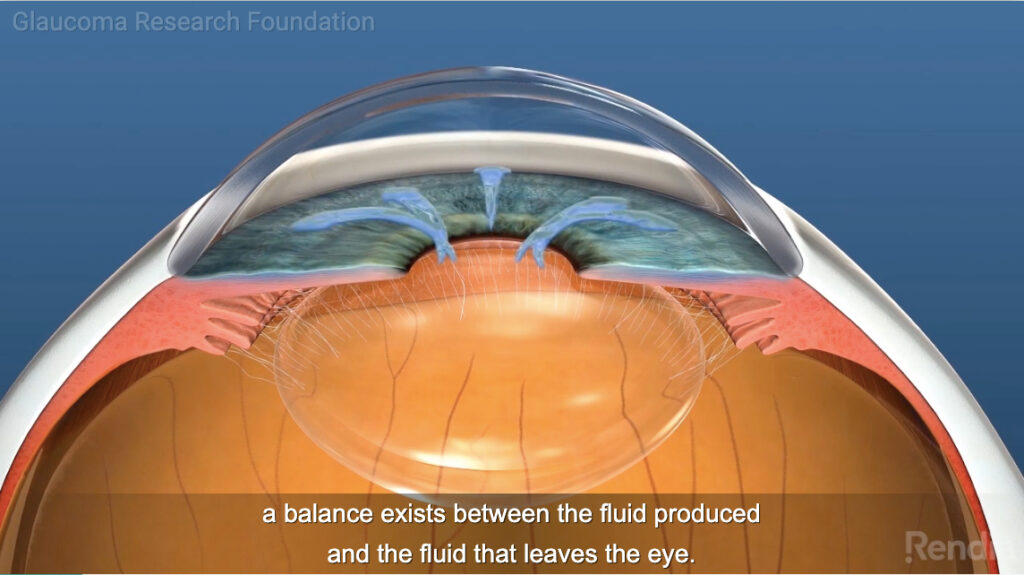
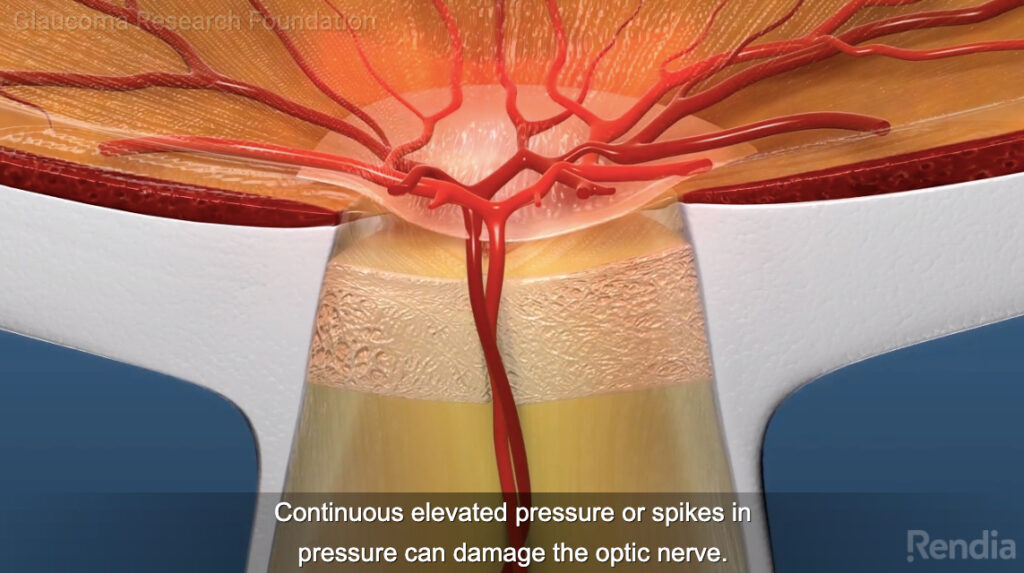
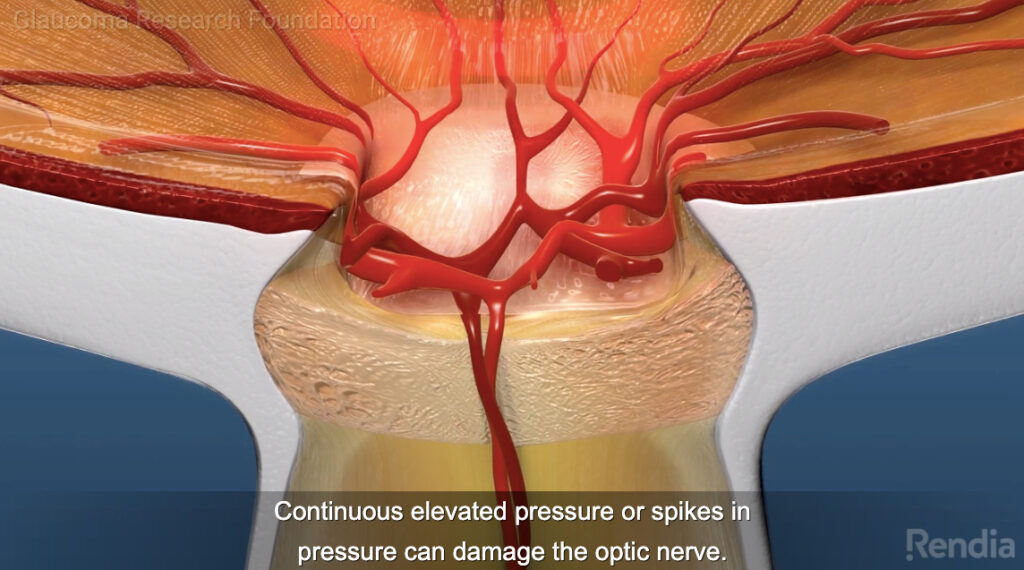
I eventually found this 8 minute series of videos. It’s by far the best overview I’ve found on the nature of the problem and approaches to treatment.
https://share.rendia.com/theater/2a2370ed-4608-4a15-4299-4c144b8a48a3
You can select one part of the series using the “◅◅1/3 ▻▻” counter at bottom left of the player.
The images at top of this page are snapshots from the second of the four parts, which is about the nature of the problem: there’s a pressure build-up in the eye, which kills part of the optic nerve. Kills, as in gone forever.
The four parts of the video:
- Your eyesight is important (duh). 57 seconds. You can skip this :)
- Excellent animated overview of what the condition is, and approaches to treatment. 1:57
- Treatments: various drops, laser surgery, “knife” surgery. 1:50.
- Types of tests they use for measuring pressure and parts of the eye
I like the clarity of the sink-and-drain metaphor in the video. But it lacks one important thing: the eyeball isn’t a sink that can overflow. It’s more like a water balloon, where bad things happen if pressure builds up.
How did this happen to me?
Updated March 15: At first I thought it might have been a complication of my botched cataract surgery last summer – I’ll write more about that story later. But glaucoma is strongly hereditary and it hit both my parents; my medical record notes “Fam hx” – shorthand for family history.
Having said that, though, my official diagnosis as of Feb 18 and again March 8 is that it was caused by steroid drops I’d been taking:
Secondary, partial steroid induced glaucoma OS, Moderate Severity
(There’s more on those terms below.)
Important update on mid-summer physician arrogance:
The glaucoma dx came from OCB, the upscale downtown Boston practice where I moved to when I lost confidence in my local practice in Nashua, after I kept having problems.
In August when I returned to the Nashua practice for a separate issue, a senior doctor there (not my regular doc) scornfully said my glaucoma could not possibly have been caused by steroid drops: “It takes MONTHS for that to start happening.” Turns out he’s wrong: more recent research says it can happen in a couple of weeks, which is what happened to me.
NEVER tolerate a doctor who’s arrogant or scornful. They have other priorities – their ego – besides your well-being.
Glaucoma is silent: it’s not normally discovered from pain or visual problems. Indeed, mine was discovered when I sought treatment for an unrelated problem, CME (cystic macular edema). (My Facebook friends can read that story here.)
On Feb 11 I saw a retina specialist at OCB, whose tests led him to promptly mark me as “suspicious for glaucoma” and changed my drops, cutting the steroid drop in half (from 4/day to 2/day) and boosting the NSAID that was intended to balance the steroid drops. On 2/18 I saw a glaucoma specialist at the same practice, who confirmed the diagnosis.
Wherever it came from, I’m stuck with it. So as always the question is, what can I do to strive for the best available outcome? It starts with learning.
Types of glaucoma
As the video above shows, pressure inside the eye is pretty much a matter of plumbing: fluid comes in, and flows out through a drain. Nearly always, nobody notices (did you know your eyes do this??), because it’s balanced and it just works, all through your life.
But there are numerous ways the balance can get thrown off – different types of glaucoma. Here’s is a simplified list. My type is “secondary” – caused by something external, not an internal condition. (Here’s the full list at glaucoma.org)
- Open angle: by far the most common.
- Angle closure: this type is a medical emergency, because you could go blind in hours. Something totally cuts off the drain, and pressure builds up quickly, and thus kills the nerve quickly.
- Secondary – caused by some accident or other external factor. (Here’s the glaucoma.org page on it.) This is the kind I have – glaucoma caused by the steroid drops I was taking four times a day.
About steroid induced glaucoma
This article is pretty lay-friendly. I imagine I’ll want to make a separate web page about this subject, in more depth, but here are some excerpts on the nature of this problem:
- “caused by increased resistance to the outflow of aqueous at the level of the trabecular meshwork … there is increased production and decreased destruction of the extracellular matrix of the trabecular meshwork.”
- The “meshwork” mentioned here is the “drain” shown in the video link at top. The eye is constantly getting a fresh supply of aqueous humor, with the old fluid draining out. The drain’s getting clogged because an excess of meshwork tissue is growing and less is wearing away. With the drain clogged, pressure builds up.
- These “cells have glucocorticoid receptors, and steroids may act on them to alter” how the system works. Aha! So that’s how it happens.
- It says only 4-6% of the population are “high responders,” having as strong a reaction as I’ve had. Still, that’s about 1 patient in 20, so it seems anytime they put a patient on steroid drops they’d need to monitor them carefully.
- “Steroid-induced glaucoma is often asymptomatic and detected incidentally by an ophthalmologist.” That’s me.
The damage so far
This ophthalmology practice does OpenNotes – I can see the detailed technical notes the clinicians type into the system. I love it. But although I can see what they wrote, that doesn’t mean it’s understandable. Example from my visit last Monday:
Secondary, partial steroid induced glaucoma OS, Moderate Severity
TMax 37, thin CCT, +Fam Hx
HVF OD ?artifact, OS dense IA
OCT RNFL OD G70, OS 57
Target: < 21 OD, < 16 OS – to be re-evaluated
IOP 29 at arrival
I won’t explain all of this (yet), but: the left eye’s RNFL (retinal nerve fiber layer) measures 57. Normal is “80-ish.” This means I’ve lost about 30% of the optic nerve in that eye. (The nerves are dead: they’re not coming back. Loss.)
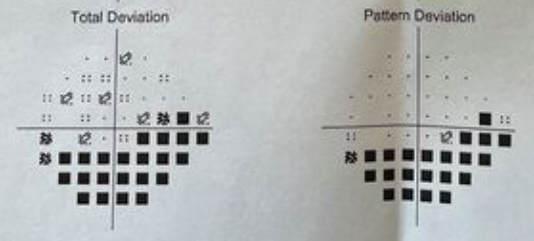
They also gladly printed out the results of my Humphrey Visual Field test (HVF). (This video shows what it’s like to take this test.) These diagrams are both for the left eye. The black squares show where I didn’t detect any test lights: I pretty much don’t see things anymore in the lower part of my left eye … even though my mind thinks I see fine, there. Peripheral vision loss, particularly looking over my left shoulder.
Current plan
As you can imagine, the treatment goal is to bring down the “IOP” – intraocular pressure. Normal range is 10-21. Mine started on 2/11 alarmingly high: 37, or 32 by a different method. (In the note above, “Tmax 37” means 37 is the highest they’ve seen. I don’t know what T stands for.)
Three eyedrops were prescribed. A week later it was down to 26, but this Monday it was back up to 29. Two more drops were prescribed. So I’m using 4 drops twice a day, and another at bedtime.
The info about each drug in this table is from this informative page on glaucoma.org (same place as the video above). Cap color is a big deal when managing a bunch of eyedrops.
Initial meds for the edema (CME):
Both started Jan 20, changed 2/11, tapering off 3/26 to end by 4/9/21
| Brand | Generic | Cap | Function | Note |
| Prolensa | bromfenac | tan | NSAID to reduce edema. $316; not on my insurance. | |
| Prednisolone (emulsion – shake before using) | pink | Corticosteroid. Like all steroids, reduces swelling (edema) by inhibiting immune system.. |
Glaucoma meds
| Brand | Generic | Cap | Function | Note |
| Cosopt | Dorzolamide / Timolol | blue | Both reduce production of fluid. D: Carbonic Anhydrase Inhibitor T: Beta blocker. | started 2/11 |
| brimonidine | purple | Decreases production of fluid and increases drainage. Alpha adrenergic agonist. | started 3/8 | |
| Xalatan | latanoprost | green | Increases the outflow of fluid. Use at bedtime. Prostaglandin. | started 3/8 |
Challenges in getting the medicine (in the eyedrops) into the eye
A huge issue, in my view, is that there is zero attention to whether the patient is skilled at getting one drop into the eye. One instruction sheet I saw said “If you’re not sure, squeeze in another one.”
I’ve come to think it’s almost scandalous that the profession doesn’t make a BIG deal of ensuring we patients know how to do eye drops successfully. If we don’t, the medicine doesn’t get into the eye, which is exactly as stupid as if it was hard to know whether you swallowed the right pills. Exactly. But there’s basically no good instruction video.
I’ve been taking eye drops for nine months (since my first, successful cataract surgery) and nobody nobody nobody, anywhere has given me a training session, especially what might go wrong if you’re not careful, causing the prescription to fail.
There’s the challenge of getting the drop (and only one drop) into the eye. Then it turns out there’s a separate problem of making sure the drop stays where it belongs for several minutes so the medicine gets inside. There’s varying advice on that, involving holding your finger on your tear duct to avoid it leaking out. But that’s hard, and the best discussion I’ve seen (the most informed and sensible) about it this on reddit:
“It can also be done by simply closing the eye. It’s equally effective as pushing the tear ducts closed with your finger.”
The discussion there links to this video on glaucoma.org, the site that continues to shine as my most useful source of information. Yet the video shows holding the bottle inches away from your face, which is nuts: for that to work, it better be perfectly straight above, or it’ll splatter on your face. (For that, the best advice I’ve seen was from a Facebook friend: rest the bottle on the bridge of your nose, with the tip over the eye.)
Additional notes to self:
- The zones of the Humphrey Visual Field test (4:40 video)
Patient communities etc
[Update Nov 9: as noted at top of this page, FitEyes is my new go-to patient group]
- Reddit r/glaucoma forum – some excellent discussions with science-minded participants and informed, supportive empathy for newcomers. Thank you, Jeanne Pinder!
- PatientsLikeMe: not much there.
- glaucoma condition page
- patient reports on glaucoma meds (very few responses)
- glaucoma search on Ear, Nose, Throat forum – very little activity, no real community
- Facebook
- Glaucoma Support (6.6k members) – good community, sane support
- Glaucoma support group (3.9k members) – haven’t been there
- There are 4 others I might try.
Status update 3/27/21
My previous update was 3/11, when the diagnosis got confirmed. On 3/26 the retina specialist did another scan and confirmed that the cyst and the edema are gone. Excellent! So he tapered the CME meds 50% (once a day now) for a final two weeks, which he says ought to reduce the pressure, and with luck maybe the pressure episode will be in the past, and I’ll just be left with one-time damage.
About eye pressure readings
I’ve become highly suspicious of my eye pressure readings. The technology to do this has changed a lot, but I also worry whether these things get checked for calibration.
- Yesterday 3/25 my left eye measured 25 in Boston, then 4 hours later it measured 18 in New Hampshire.
- The New Hampshire practice had, the week before, measured that eye with three different devices, getting readings of 8, 11, and 13. (Normal is about 10-21!)
- In Boston the week before that, it was 29 then 27.
It seems quite unlikely that I’d bounce from 27 down to 13 then back up to 25 in Boston but 18 a few hours later in New Hampshire. I’m going to ask around about this on my patient forums.
Next step: see the glaucoma specialist on April 6.
The problem of preservatives in eye drops
Turns out the surface of my eye is mighty sensitive to the preservatives used in eye drops to keep them from growing bacteria. (Dropping bacteria into the eye is, um, not recommended.) My eyes started to burn, itch, ugh. It turns out this was caused by preservatives: when we switched to preservative-free (“PF”) drops the problem shrank 90% almost overnight. (We did that for 3 of my 4 drops; the other is insanely expensive for PF so I’m using over-the-counter artificial tears (preservative-free Thera-Tears) to soothe them. As of this writing 6/25 I’ve barely needed any for a couple of weeks.
This seems to be an informative article about preservative issues: Preservative-Free Alternatives: Options for decreasing ocular toxicity in patients with glaucoma. Caveat: I haven’t check it yet with any trusted sources, and it’s five years old. Ugh:
Unfortunately, most preservatives in ophthalmic medications disrupt the ocular surface and [aggravate any existing problems with the surface of tye eye, e.g. dry eye.]
Benzalkonium chloride (BAK) is the most widely used preservative in antihypertensive topical medicines, and many studies have clearly demonstrated BAK’s toxic effects on [the surface of the eye].
Arg!
But the article has a priceless quote that shows signs of patient-centered thinking:
Reducing patients’ overall preservative load may improve adherence, [y’think?? if the drops cause pain, I might not take ’em??], quality of life [duh … reducing the itch may improve my quality of life????] and the patient-doctor relationship” [thank you for saying that!]

A big issue with anything PF (prescription or not) is that to keep the drops sealed from contamination, they don’t come in the usual bottle: they come in little plastic “single use” tubes (“vials”). After twisting off the cap and squeezing out one dose, you’re supposed to throw the rest away.
Individual vials cost more, of course. PF TheraTears on Amazon are about 33c/dose; it’s hard to compare unit prices with ordinary bottles, because I can’t find out how many doses you’re supposed to get out of a $13 bottle of drops.


On Reddit, a user posted:
“This is beautiful! My dad is suffering from Glaucoma and we’ve really just learned alot through articles and people’s experience. It’s great to have that a self education page like this one. Such a convenient addition.”
I’m on the FitEyes mailing list (relatively new, haven’t contributed). Just wanted to say how informative and well-written your site is. And it’s nice to have someone agree with my thought that basing treatment decisions solely on one random pressure reading every few months makes zero sense.
Hi Mark – I assume you mean the FitEyes site?