Caution: This post is not a prediction. It’s just a tutorial about the concept of herd immunity, with an eye to why it’s probably not an approach the US wants to take in solving the complex problems we’ve gotten ourselves into with COVID-19.
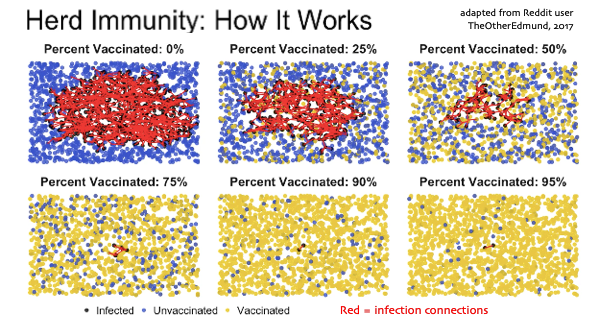
Click this graphic to go see a six second animation of these images, created in 2017 by Reddit user TheOtherEdmund. You many need to watch a few times. Get a feel for the differences in what happens in the different blocks, and come back to discuss:
This weekend I’ve labored to understand this concept, which first came to my ears regarding coronavirus in March, when British prime minister Boris Johnson proposed it as a possible approach for Britain to take: let the virus take its course, and they’d end up with “herd immunity,” and that would be the end of that.
In my unsophisticated knowledge “herd immunity” meant “you let the weak cows die, and the rest of the herd will be fine.” And in fact in April a Tennessee protestor held up a sign saying “Sacrifice the Weak – Reopen TN.” (It’s not clear whether the sign was mocking or real (Snopes), but it illustrates the point.)
But it turns out there’s a lot more to the concept than just “sacrifice the weak.” There’s a specific way herd immunity works – and it does work for things like measles and mumps and polio, via vaccines. But in the absence of a vaccine, it’s an absolute disaster.
Here’s why. Here’s a snapshot from the start of the animation.
- Each blue dot is a healthy uninfected person – you.
- Each yellow dot is someone who’s immune – “can’t touch this,” if you’re into MC Hammer.
- Each red line is where someone uninfected crossed paths with an infected person and got infected – an “infection connection.”
- Notice: the more people get vaccinated, the fewer red lines happen. Vaccines prevent infection – who knew??
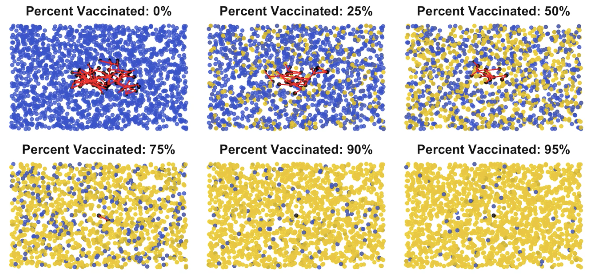
As time goes by (in the animation and during an epidemic), here’s what it looks like a while later.
If nobody is vaccinated, the disease spreads pretty rapidly; as more of the population is vaccinated (more yellow dots), the frequency of new red lines drops dramatically.
The explosion of infections among the unprotected is exactly what happened before vaccines. Epidemics were rampant and unstoppable.
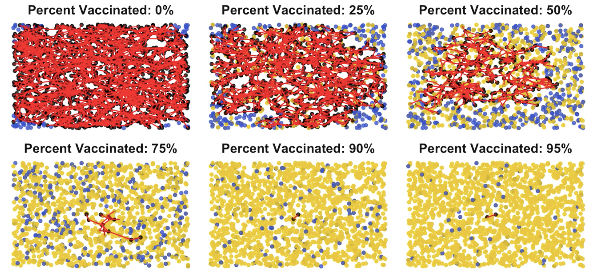
And here’s what it’s like at the end of this animation (though in real life it doesn’t stop):
See how around 90% in this example there are nearly no infection connections – few red lines? For any given disease situation, this point is called the herd immunity threshold. When you get to this many yellow dots, it’s manageable. Hospitals aren’t overwhelmed, and you can do contact tracing, as South Korea and others do: you can hunt down every single remaining case and find out everyone they contacted. In other words, you can find and protect the blue uninfected dots … and you can stamp out the disease.
Of course there are a zillion variables that change the speed: how contagious is it? (Each mumps patient infects 10-12 others; each polio patient infects 5-6 others, etc. This is what’s called the “R” number, for reproduction.) How tightly packed is the population? (It’s believed that New York’s crammed subway system was a major factor in the early explosion.) Etc.
Regardless of the variables, that’s the basic concept. (For coronavirus the R number is around 3, and the herd immunity threshold is tentatively believed to be somewhere around 60%.)
But here’s the problem:
We ain’t got no vaccines.
So we’re stuck at “0% vaccinated.”
That’s why, everyplace the virus shows up, it spreads. It surprises everyone, because at first it’s slow, because infected people are invisible for days or weeks (which is why forehead thermometers are not enough), so it’s spreading silently. Then BOOM, a certain percentage get sick. And by that time it’s spread all over the place.
It’s not unlike a wildfire that spreads underground. By the time it erupts, you’ve got a widespread problem on your hands. And the longer you take to notice it and start fighting, the bigger a problem it has become. Which is exactly what happened in the US. (Nobody disputes this; the only argument is whom to blame, but that won’t save your life or mine.)
The other approach: get infected and survive.
Here’s where we get to the COVID-19 version of the story.
There’s another way for a herd to be immune, aside from vaccines: have a lot of critters get sick. Some die, and the rest develop antibodies.
This doesn’t always work – we don’t know yet whether COVID-19 survivors are immune, because the disease is too new. Plus, it’s a new coronavirus (“novel,” as they say); other coronaviruses are one cause of the common cold, which people get year after year – there’s no immunity and no vaccine. (If you’re thinking “Yikes!!”, that’s appropriate.) But no cold virus has ever been fatal before, so we didn’t have much motivation to solve it.
There have been two killer coronaviruses: (Thanks to Bill Reenstra and Stephen Owades for pointing to these, which I’d overlooked in the original post.)
- SARS-COV-1 infected only 8,000 people, killing 774 (about 10%), and was contained in 7½ months.
- MERS has never stopped but is rare. Since arising in 2012 it’s infected 2,519 people, killing 35% of them (866 deaths so far).
Of course we hope the urgency, extreme spread, and enormous death count of COVID-19 will motivate immense investments to achieve new things.
Update next day: But while I was working on this post, CNN Health posted an informative article, What happens if a coronavirus vaccine is never developed? It’s happened before. It quotes British Covid-19 expert Dr David Nabarro: “It’s absolutely essential that all societies everywhere get themselves into a position where they are able to defend against the coronavirus as a constant threat, and to be able to go about social life and economic activity with the virus in our midst.”
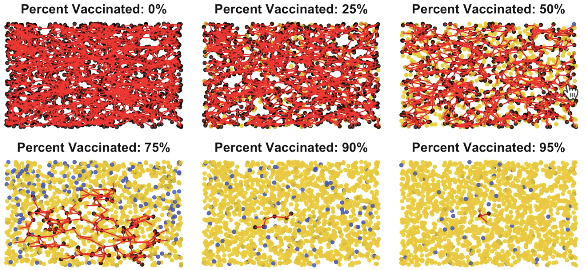
In any case, instead of each of these diagrams being labeled “vaccinated,” our reality today is that each yellow dot doesn’t mean “vaccinated,” it means “got infected & survived”:
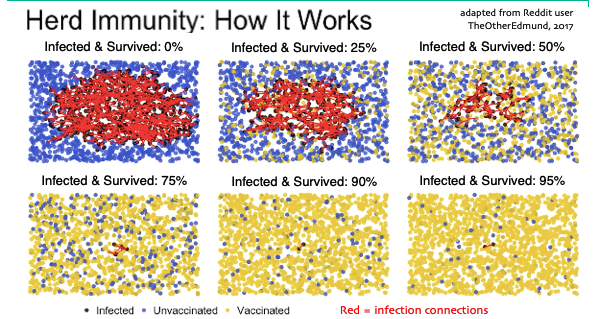
Ha ha look how funny – this particular image shows herd immunity kicking in after 75% of the population has gotten infected. In the USA that would be 75% of 328 million is 246 million infected people. Ha! Ha!
That includes 75% of everyone you know getting infected. Including, probably, you! Ha! Ha!
And since our best estimate is that 0.5% to 1% of all infections for this virus die, that would be anywhere from 1.23 million to 2.46 million US deaths. What a laugh riot!
(Again, these are not exact numbers; they’re just to convey the principle. But they are in the right ballpark.) (And by the way, in these diagrams, each dot represents around 400,000 Americans.)
A herd immunity policy without vaccines is mass murder. And worse.
It’s not just mass murder; it’s a whole lot of very sick people. A friend had the virus and had a fever of 103 for ten 23 days (then 101 for a few more). She was suffering, and of course with this damn virus there’s the always-present fear: “Will I be one of those who suddenly goes downhill fast and dies?” Think about living that way for weeks – both you and your family.
Whoever cares for those very sick people – a relative or a professional – is vulnerable to getting sick, too. More than 200 doctors and nurses had died by April 10 – and last week the stress caused two different New York professionals to commit suicide: a top ER doc and a newly minted EMT, months out of training. And Peter Elias MD wrote on Facebook, “The data I have seen is in the range of 1 in 10 to 1 in 5 household members or caregivers.” (Update: Peter commented that a doc on Twitter posted an informative summary of 14 recent papers on this; I summarized below.)
Imagine all that happening to half the country’s population.
Your only way out: Avoid contact! Wear masks! Wash your damn hands!
We will, someday, have vaccines or at least treatments. (Either that or the world is ending.) Remember, all those diagrams in the animation have variables, and a big one for this virus is how often people bump into each other – literally or figuratively.
Another big variable, when they do cross paths, is whether the virus passes between them and enters the other one’s body, causing a new infection. That’s where distancing, masks, and hand washing come in. They are our only defense right now – but they work.
Avoid getting or spraying the virus. Either you or the other guy may be the sprayer – there’s no way to know. Just be responsible. And every time you come home from outside, wash your hands for “two happy birthdays.” The soap bubbles break open the little virus cases, and poof, they lose their power. Just with soap!
You are not powerless against this bugger. You just gotta do it and keep doing it. Maybe for a year or two. Just avoid being either end of a red-line infection connection.
The more we slow down that animation, the better the chance the geniuses will invent effective medicines before that red line knocks on your door.
Be responsible in your community.
Stop the spread, and spread the word:
Tell people “It’s not just me. I don’t wanna kill a nurse.”
And if anyone suggests herd immunity, please show them this. I’ve had smart scientific people check it, and this is true. Herd immunity is fine with vaccines. We ain’t got one.
Additional resources
- Here’s Why Herd Immunity Won’t Save Us From The COVID-19 Pandemic – a good, concise, clear and accurate article on ScienceAlert
- What the Proponents of ‘Natural’ Herd Immunity Don’t Say (NYTimes)
- A 2014 Nova piece on herd immunity
- For the nerdy, a surprisingly readable economics policy paper from April 24 discussing different ways to look at the overall COVID-19 problem, including herd immunity as one option. (47 page PDF, but really understandable … if you skip the stuff that’s hard to understand.)


Very good analysis. There have been deadly coronaviruses think SARS and MERS.
The other issue with recovering from Covid19 is that there maybe long term health issues. Hopefully, if they exist they are more like mumps than polio.
Thanks for reminding me about SARS and MERS! Duh.
What a weird “family.” Some benign but annoying, some absolutely toxic.
Great post. Thanks.
I would avoid the term ‘likely’ to describe infection risk in family and caregivers. It is too vague. Certainly, infection in a household contact or caregiver is more likely than in someone who only has intermittent or casual community contact, but some will interpret ‘likely’ as ‘probably’ and that – based on current data – is wrong.
We don’t know for sure, but the current data I have seen suggests that transmission rates among caregivers and within households is 10-20%. I’m sure these estimates are approximate and will change with newer and more robust data.
This study suggests 10% transmission in household contacts:
https://www.medrxiv.org/content/10.1101/2020.03.24.20042606v1
This claims 20%:
https://www.webmd.com/lung/news/20200430/covid-19-household-spread-how-likely
Thanks, Peter! Since you first said this in email and FB, I edited the post to fix my error. Much appreciated.
SARS and MERS are both coronavirus diseases with pretty high fatality rates. They seem to have receded after initial outbreaks, reducing the need for a vaccine. But some of the work on a MERS vaccine is giving researchers a leg up on a COVID-19 vaccine.
Thank you. Please have a look at the addition I made (search MERS) and if it’s not adequate please let me know.
Yes, in Minnesota we are not going for any herd protocol. We do not need to do anything for the whole state when 70% of all deaths from COVID-19 are taking place in nursing homes and assisted-living facilities. Another large percentage catch the disease because they work in meat-packing industries with very close quarters. We can focus on these known places where the disease is thriving. And the rest of us can soon get back to our normal lives. I do not expect that a large percentage of Minnesotans will ever get this disease.
Correction: in the original post I wrongly said coronaviruses don’t kill people. Sloppy. Bill and Stephen above pointed out that the SARS and MERS viruses did. So I added the following:
________
But no cold virus has ever been fatal before, so we didn’t have much motivation to solve it.
There have been two killer coronaviruses:
– SARS-COV-1 infected only 8,000 people, killing 774 (about 10%), and was contained in 7½ months.
– MERS has never stopped but is rare. Since arising in 2012 it’s infected 2,519 people, killing 35% of them (866 deaths so far).
A cold is a collection of symptoms – coughing, sneezing, a runny nose, tiredness and perhaps a fever – rather than a defined disease and yes people can die from any number of other viruses.
The flu which is also caused by a coronavirus for example also kills people. “This season CDC estimates that, as of mid-March, between 29,000 and 59,000 have died due to influenza illnesses”
That isn’t to say that coronavirus is the same as the flu (just that other coronavirus do in fact kill people). https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-disease-2019-vs-the-flu
Another correction: I had wrongly said in-home caregivers are likely to get the virus. I’ve edited it to better match Peter Elias’s comment: the post now says they’re vulnerable. (Peter’s links say somewhere between 5-10% get infected.)
Update: see Peter’s comment the next day, below, for a lot more detail.
Someone had to analyse this and write it up in a readable way. My son really like it too so double thanks from Godzone.
As life and luck would have it, a thread appeared in my Twitter stream this morning summarizing infection rates among close contacts. Here is the threadroll:
https://threadreaderapp.com/thread/1257392347010215947.html
That’s a terrific review of 14 studies in many countries. Thank you!
I’ll paste in the conclusions. (Note, all, these are PRELIMINARY and suggestions of things that may or may not turn out valid with further study. I’m posting these to stimulate thought, to illustrate what science looks like when it’s in process, and (for me) to start fleshing out a picture of what life may look like with constant rolling COVID-19 outbreaks as life moves forward.
_________
The tweeter is Dr Muge Cevik (MD, MSc), virologist at the Univ of St Andrews in Ediburgh.
Opening tweet:
“A lot of discussion recently about transmission dynamics, most of which are extrapolated from viral loads & estimates. What does contact tracing/community testing data tell us about actual probability of #COVID19 transmission(infection rate), high risk environments/age?”
She then presents 14 papers from early March up to last week, with a variety of findings. Summary:
_______
/15 … these studies indicate that close & prolonged contact is required for #COVID19 transmission. The risk is highest in enclosed environments; household, long-term care facilities and public transport.
__________
/16 High infection rates seen in household, friend & family gatherings, transport suggest that closed contacts in congregation is likely the key driver of productive transmission. Casual, short interactions are not the main driver of the epidemic though keep social distancing!
17/ Increased rates of infection seen in enclosed & connected environments is in keeping with high infection rates seen in megacities, deprived areas, shelters. A recent preprint demonstrates that #COVID19 epidemic intensity is strongly shaped by crowding
18/ Although limited, these studies so far indicate that susceptibility to infection increases with age (highest >60y) and growing evidence suggests children are less susceptible, are infrequently responsible for household transmission, are not the main drivers of this epidemic.
19/ Finally, these studies indicate that most transmission is caused by close contact with a symptomatic case, highest risk within first 5d of symptoms. To note: this preprint suggests that most infections are not asymptomatic during infection
https://www.medrxiv.org/content/10.1101/2020.04.25.20079103v1
In conclusion, contact tracing data is crucial to understand real transmission dynamics.
Cautionary note: This data & interpretation is based on the available evidence as of May 4th. Our understanding might change based on community testing/lifting lockdown measures.
Addendum: While we have limited data, similar high risk transmission pattern could be seen in other crowded & connected indoor environments such as crowded office spaces, other workplace environment, packed restaurants/cafes, cramped apartment buildings etc.
Conclusion 2:
(a) we need to redesign our living/working spaces & rethink how to provide better, ventilated living/working environment for those who live in deprived & cramped areas;
(b) avoid close, sustained contact indoors & in public transport, & maintain personal hygiene.
I continue to make corrections or additions as I find them. The friend I cited who had the virus says the 103 fever lasted 23 days, not ten, with another few days at 101, at the end. That’s almost four weeks straight. Ow.
Note, btw, that said friend was told that this case did not qualify for testing – and when testing was allowed, hallway conversations revealed that the hospital was under pressure to not report a lot of new cases, for political reasons. But that’s a separate issue from herd immunity.
Oddly, this post is getting stolen and cross-posted by pirate bloggers. I’m going to keep a list of them here. I’ve had this happen rarely in the past but not this much.
adekstore[dot]com/the-problem-with-herd-immunity-as-a-covid-19-strategy/
floydneilltechnoblog.wordpress[dot]com/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
lauramalchow.wordpress[dot]com/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
healtheconbot.wordpress[dot]com/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
brighterlifepage.wordpress[dot]com/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
healthadviceandmore.wordpress[dot]com/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
safetyhealthnews[dot]com/the-problem-with-herd-immunity-as-a-covid-19-strategy/
healthfacts[dot]online/index.php/2020/05/05/the-problem-with-herd-immunity-as-a-covid-19-strategy/
ozfeed[dot]com.au/2020/05/06/the-problem-with-herd-immunity-as-a-covid-19-strategy-ozfeed-medicine/