Sometimes I don’t know where to post something – on e-patients.net or here. My dividing line is usually: if it’s specifically about participatory medicine, it goes there; if it’s about my views about healthcare in general as someone who goes to a lot of meetings, or specifically about patient engagement, it goes here. This one’s both; I posted it on the e-patient blog, but I want it on this archive too.
________________
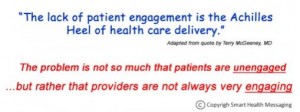
Over on Mind The Gap, Steve Wilkins (Twitter) has a poster about patient engagement that annoyed me:-) right out of the box – because although I pretty much like everything he does, the poster starts with what I find to be the ouchiest mental disconnect in all of medicine today. But it quickly follows with the flipside. Here’s a screen grab from its top:
Gut reaction to first quote: What?? “The lack of patient engagement is the Achilles Heel of health care delivery”?? Shades of Health Leaders magazine last October, which said – in an issue on Engaging the Patient no less! –
In our annual Industry Survey, leaders cite patient noncompliance and lack of responsibility as the fifth-greatest driver of healthcare costs … a quarter of respondents pointed to patients as among the top three cost drivers, ahead of health plan overhead, medical devices, pharmaceuticals, and malpractice litigation.
I love it – patient satisfaction scores are generally mediocre, 1 in 70 Medicare admissions ends in accidental death (Inspector General, Nov 2010), and the people who run these chop shops blame costs on their slacker customers. Sounds like scapegoating to me!
And this is the magazine whose September 2009 cover story was “Patient of the Future,” about e-patients, and whose Dec. 2010 “Twenty People Who Make Healthcare Better” cited two SPM founders. (Re the survey, don’t blame the messenger (the editors) for their readers’ views. The magazine does know how to hear its customers!)
I don’t know Dr. McGeeney (author of that quote in the poster) (I’d love to meet him/her), but holy cow, Achilles heel? How about access to care, disparities, cost of care, listening to what patients value, etc? It’s particularly perverse to have a system where care is unaffordable to many, or hard to get to, and then assert that the problem is that patient engagement is the Achilles heel of care delivery.
I recently heard a prominent executive say “One of the dragons we need to slay is the idea that care should be convenient.” I’m not kidding.
But then:
Second quote: “The problem’s not so much that patients are unengaged but that providers aren’t always very engaging.” Ahhh, thank goodness: it’s a partnership! Who knew??
The poster goes on to list many items that cause trouble on the front lines: harried practitioners, interrupting, etc etc. All valid points.
My favorite, visually, is this cartoon. (All clinicians aren’t like this! None of mine are, for sure. This is a cartoon that effectively depicts a common problem, not a universal one.)
So, before coming over here to write this, I dumped this comment on Steve’s post:
I need to write something about the dimensions of patient engagement.
To a lot of people it’s a synonym for compliance – obedience. In my experience many observers of healthcare see *many* patients not following instructions and conclude “[all] patients are not engaged.” In the observed cases that may be accurate but in my experience too often this blinds the observer to a useful question: what can be done to *interest* the patient in doing more good things?
A common issue, again in my experience, is that in many cases the goals are imposed by the clinician. That makes no more sense than a financial advisor saying “You should be saving 20%. You’re non-compliant.” Note, I’m not disagreeing with the principle or the evidence here; I’m just saying, let’s do things that WORK, let’s FIND approaches that work.
AND, as another layer, activated e-patients who want to redesign the care system feel that the system itself is pretty frickin’ non-responsive, I might add. :-) The huge difference is that we the patients are the BUYERS of services done to us (usually through our insurance), so it’s odd and perverse when some providers not to ask what WE want, individually and collectively.
And that, I suspect, is a root issue in exploring what “patient centered care” is.
So now I gotta email you about your patient engagement white paper to see whether you agree. :-)
====
p.s. Steve and everyone, can we please stop calling every data poster an “infographic”?? A poster like this is a dressed-up presentation of a bunch of facts. It’s nice; it’s a more enjoyable way to absorb facts than a row of numbers. But to me an infographic is when the graphic adds information, rather than just dressing it up.
Example: in this, from Misfitwearables.com, the layout makes it easier to understand the data, not just to read it: the layout shows the relative position of each sport on two scales at once – cost of getting into it, and caloric benefit. (2020 update: see what became of Misfit.)
For instance, running is on the cheap inner circle, cost-wise, and on the rich calorie-burn circle; equestrian is expensive and doesn’t burn much. See how the layout helps you see the relationships among the data points?
As Edward Tufte pointed out long ago, useful data visualizations are multivariate – they depict several things at once. That’s how the graphic adds information – it shows the relationship between data points, not just the data points themselves.
And that helps people understand things. And that’s a good thing.




Leave a Reply