 Glossary for non-English readers: “ratty” = poor condition; boxers = boxer shorts (Wikipedia).
Glossary for non-English readers: “ratty” = poor condition; boxers = boxer shorts (Wikipedia).
This is an update on a post from three years ago about the business of patient engagement – the challenges of starting a business without funding or a proven business model. As regular readers know, after years of struggle I turned an important corner (my business reached break-even), and looking back, I want to explain something.
Back then my underwear included ratty boxer shorts. (I took a picture but you don’t want to see it.) In the face of my other bills, I couldn’t afford to buy new underwear. Yet time after time people invited me to come…
- speak for free
- advise their company for free on the phone
- attend policy meetings for free.
Some even asked me to pay my own travel costs. See the recent post A turning point for patient voices, which details the irony in telling someone their voice is valuable but then saying it’s not worth spending a cent.
(Others did offer support, even for advice by phone. Early examples who come to mind include Emmi Solutions and InfoSurge – importantly, both are patient education companies!)
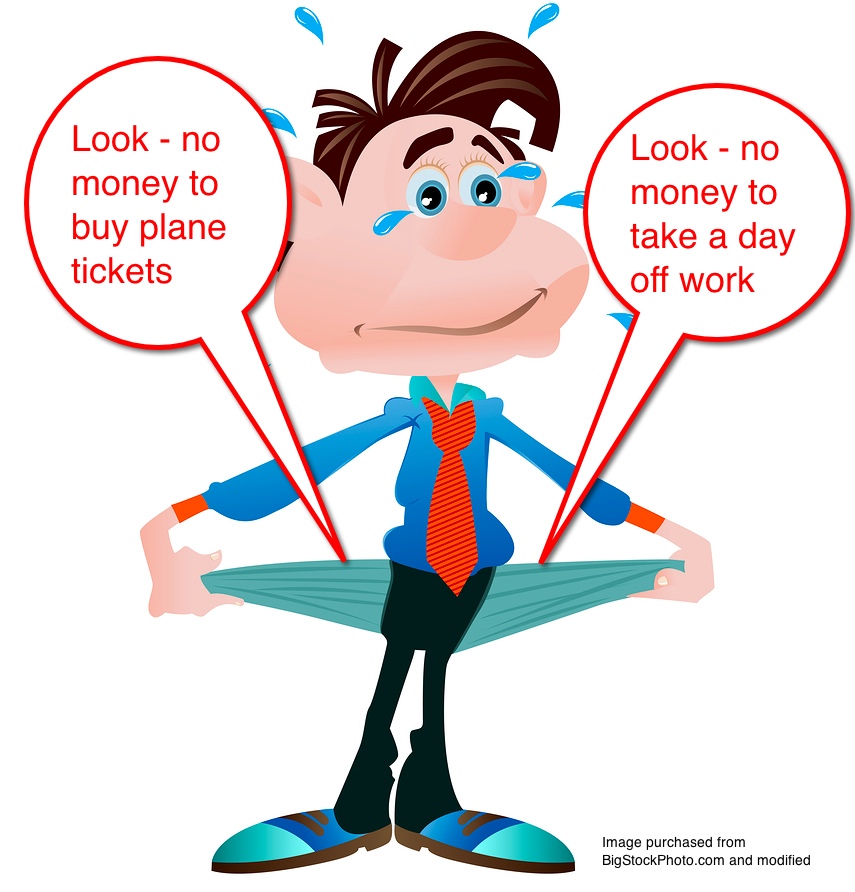
Like many experienced patients, back then I had plenty to say but I didn’t have any money. To attend an event and contribute value, I needed funding . I was the same person I am today – I just didn’t have any money. And I couldn’t spend money I didn’t have – I was being responsible.
How ironic that being responsible would squelch a patient.
Here’s the trap: it’s become clear to me that folks think people who are short on cash must be incompetent: “They’re poor for a reason” – so what good could their opinions be? That’s ironic because the most experienced patients tend to have the most front-line experience.
Have you ever had no money?
In a skit long ago, comedian Flip Wilson said “It’s hard to sing the blues when you’re pretty much doin’ all right!” A similar problem seems to affect people who have good jobs in the industry so they can’t imagine what “no money” means to patients, and would rather not think about it.
Heck, just before my cancer diagnosis I remember getting a $25 restaurant gift card and getting two meals each out of it, for my wife and me.
Again, I have no complaints. I’ve never been rich, but I’ve been comfortable all my life – until this happened. And some years back I myself couldn’t understand how some people could be thrilled when they got new underwear for Christmas. Now I know.
A year or two back one conference company, World Congress, talked to me for an hour about whom to invite to a new conference, then told me they had no intention of hiring me – they were just getting free consultation. (It’s one thing when a conference asks relevant speakers to speak for free; it’s even worse when they don’t know whom to invite! But that’s the company’s business model: get somebody to dream something up, get others to contribute content, and get others to come pay for it.)
It’s a mistake to think someone who can’t donate their time must be stupid.
I want you – all of you in healthcare and government and health policy who are “pretty much doin’ all right” – to understand: This is what some patients’ lives are like – especially the sickest, most experienced patients. Yes, medicine does need to hear patient voices, and no, we can’t just ask them to donate their time. You may find it hard to imagine, but it’s true. Think about it, and believe it.
From the bottom of my heart, I thank the people who supported me in those early days. Thank you, thank you, thank you.


Many Moms like me find themselves single and unable to work full-time due to their child’s extraordinary medical needs. I became “Hand Me Down Rose.” We even found ourselves at our church’s food pantry a couple of times.
My marketing and communication background was sought after to help understand the patient experience. When I pointed out that other professionals were paid more for the same level of expertise, I was told I was paid for my experience as a family member – not a University Professor in business, marketing and communications.
Sadly, many organizations do not see a value in anyone who does not have a medical background. Fortunately, in no small part due to you and other’s pioneering the way, some healthcare organizations understand the importance of the patient and family voice and appropriate compensation for time and expertise!
And let’s acknowledge with gratitude organizations like Cautious Patient Foundation, Partnership With Patients, Society for Participatory Medicine, and IHI for either directly funding or materially supporting citizen-patients over the past several years by providing, by one means or another, travel funds for patient “activists” to gather in Orlando and Kansas City.
For organizations or meeting planners wondering about bringing in citizen/patient voices and paying for them, I’m sure that engaging in typical due diligence to scope a prospective participant/speaker’s work will help assess an individual’s suitability for any given event.
Absolutely, Bart! Thanks – for more than a year I’ve wanted to start generating a list like that of the pioneers of support for the patient voice.
Can anyone name some others?
Hmm: sometimes it’s not “no money” as in broke or poverty-stricken; sometimes it’s “no money” to redirect from retirement safety net despite one’s deep desire to improve everyone’s experience in health treatment, citizen and provider alike.
Yes yes. What you note is related to my comment about “amid my other bills.”
In my view it’s no better to say “C’mon, donate some of your retirement money to our event” than it is to say “Donate some of your grocery money.” It all amounts to “Bleed a little for us, will ya?”
And the point of this post is that to people who are “basically doin’ okay” it’s hard to imagine that. And perhaps those people are in a perilous role if they try to guide healthcare?
If I ever do break into that speaking circuit I’m going to ask for as much as that accredited neurologist that knows much less than I do about the exact same subject.
Dean, I hear you, but as we’ve discussed in this site’s Speaker Academy series, there’s more to getting paid than just deserving it – in practical reality it’s necessary to earn a reputation.
Clinicians sorta GET one, by the credentials after their name. We know those credentials may or may not guarantee reliable authority but that fact’s not useful if one’s trying to get paid by the people inside the system! :)
Sing it, brudda – you know I know *exactly* what you mean. I’ve long suffered from Ratty Underwear Syndrome, in clear violation of my Nana’s Rules on such (NEVER wear anything out of the house that you wouldn’t want seen by an ambulance crew!) – I started refusing to work, or speak, for free a couple of years ago, since I figured giving up “opportunities” that were putting me at risk of living in my car were easily turned down.
I have earned my reputation by delivering value when and wherever I was given the chance to – it’s now up to me (and to all of us) to make sure we start putting a price tag on that value. It’s a rising tide/all boats scenario.
Clearly, your time has come. We all are grateful to you for carrying our banner!
OMG – well, I guess this shows there’s something for EVERY cause on the interwebs: Holes In Your Boxers on FanPop.
I read your blog entry right after reading a physician’s about how patients really don’t seem that interested in engagement. The anonymous doc cited his experience of giving email, website, Twitter and Facebook access to his patients and they really didn’t seem all that interested. Therefore, his conclusion was.. patients really aren’t as engaged with their healthcare as everyone thinks they are and so by extension, we really shouldn’t care so much about patient engagement. I thought my head would explode at the dissonance and disconnect. The potential polarization and ownership by medical professionals of who cares and who doesn’t feels very dangerous to me. At the same time I know many providers who really want to engage but are really not sure how. (I know.. I know..)This generated two ideas:
1)Kick or Med start funding to organize and maintain a patient registry for all those interested in speaking or consulting. I realize that there are issues with an open registry but I also would encourage not being afraid of inviting all voices to be heard. Some of the most powerful and insightful teachings about healing in my life as a nurse practitioner have come from sources like my friend with Down’s Syndrome or my many clients with schizophrenia. As a non-doctorate prepared academic and a non-physician primary care provider, my “cred” is brought into question regularly so I understand the fear. I do think it’s worth pushing past and opening to all. You never know what magic might happen and there sure is power in numbers! You could divide the registry by “specialty” and potentially use a rating system like Klout scoring to highlight the most influential or sought after and at the same time making a place where all are welcome. In addition to the registry.. creating a pricing guideline: per hour, per event, etc. etc. you could work out many possible recommended price points. This would allow registered patient speakers a point of reference when negotiating an engagement and allow health care organizations a reference when they budget for events or project brain storming or system planning etc. where they desire patient input. And.. maybe you or someone you know has already done this :) I realize I’m coming late into an ongoing conversation..
2) Kick or Med Start funding to develop a practice guideline for providers regarding patient engagement and empowerment. I really feel for my colleagues who want to do something and simply don’t know where to start. And while it’s easier and feels better, even for me, to say DUH! it’s more productive to tell them how. If patients don’t do this, some provider or organization will write their own eventually and then we’re back to square one. I’m pretty sure we don’t want the AHRQ doing this!
So thanks Dave for giving voice to so many who feel silenced and thanks for poking me to do this on the blog. Now you understand why I fumbled my way through Twitter!! I need way more than 100+ characters..
Lots to say on this, but first – for comparison, got a link to that physician blog??
In my experience there are a lot of patients who indeed don’t even know what it would look like to be engaged and empowered. This exactly parallels the way many women in the 1950s couldn’t imagine what it would be like to be a CEO or even to have girls’ sports in school.
We all need to be careful not to take current mainstream as the definition of what’s possible or appropriate. And we all need to be careful not to assume that one who does think that way can’t change when they see a new light.
Showing them a new light is one of the key aspects of our work.
Dave, You’ve hit my Twitter weak spot.. I read and read and then forget where I read it unless I send it to myself. I cant say for sure but I believe it was an anonymous physician reply to a blog post by @medrants. I’ve been consuming information, feeding my own brain. I’ll start paying closer attention to references!
Let it never be said that I take current mainstream as the definition of what’s possible or appropriate :) I’m in!
Speaking of seeing the light..I’ve been trying to influence the conversation in the current drama around the Physician vs NP debate fueled by the large primary care medical organizations. Playing with the idea of creating a movement around #can’t we all just get along. I’m not even sure if there are supposed to be spaces between the words of hashtags LOL
Vis a vis your blogs about professional services, a relative by marriage of my husband, whom I met exactly once, at a funeral, asked what kind of writing I do. Then of course he said he has an idea for a book but can’t get focused, but would I read it — not proofread it, his wife can do that, but just maybe make suggestions. I was going to talk my way out of it but my husband said it’s his relative and he’d read it, so now we both have to, I guess, if he ever gets around to writing it. After all, it will only be maybe 100-150 pages. Nothing at all.
Well there you have it! Nothing at all!
Of course in MY view, nobody “has to” do anything – to say that is, in my view, to express powerlessness.
A good friend has been trying to teach me for years to teach me to say “I’m sorry – my schedule won’t allow it right now / anytime soon. Good luck!”
Update: Empowerment is contagious.. I spent 30 mins yesterday on the phone with the PA Bar Institute convincing them that the parents of exceptional children and the exceptional children themselves should be invited gratis to their conference “Exceptional Children Conference2013”
The current rate for family and child to attend is $200 per person. Expecting a phone call back today to continue the conversation about scholarships. As the worlds of medicine and law continue to collide vis a vis the ACA, big data and privacy issues and state regulations, representing the patient voice in the world of law remains an important priority.
YOU MUST GO THE WEB SITE TO SEE THE HILARIOUS PIE CHARTS. http://www.27bslash6.com/p2p2.html
[Edited by Dave – It’s a long email exchange, sometimes obscene, between an artist and a client who’s trying to suck more free work out of him]
Oh, e-E-Patient Dave deBronkart….you have no idea what a trigger that is for ME as well….I don’t have ratty boxers as a visual image of my poverty….but thank god I’m on TPN cuz I’d still be dumpster diving for food otherwise…and organizations used to ask me all the time to “speak for free”, write for them at no charge “cuz ur a pt”, or fly to WDC at my expense to “lobby”….and when I finally presented my resume for a JOB, was told I was too “sick” to work….really?
Great comment, Patricia – but what’s TPN?
TPN = Total Parenteral Nutrition. In plain English, feeding via central line or catheter. Medline page: http://www.nlm.nih.gov/medlineplus/druginfo/meds/a601166.html
Patricia, I also used to be on TPN, and attended a meeting held by AusPEN, first they waited until I paid my registration then asked me to present a talk.. I organised my talk for 20min and yes used my money to do handouts, and the usual PPP as it was in those days.[ around 2008] I thought I might get a rebate when I arrived but no. first they swapped the time of my talking about being on PN, then asked me to drop it by 10min as the first speaker went over by 20min.. no one else was asked BTW, then I got interrupted at the 3min mark to say that they needed to really catch up and everyone wanted their lunch so please cut it further. YUP I did know how to do talks Id done them as a nurse.. so my last minute I changed everything and said how it stunk to be on PN that the care was missing, that no patient input was ever asked and we had to blend in with the compounding pharmacy to have ingredients that suited them so they could make up batches of feeds, and no individual ones. FUNNY they removed my name off the mailing list for any further meetings.
At the afternoon tea break I was spoken to by several conference delegates, who were sad that I had not been given my time as they had hoped to get ideas for their own patients. so we had a quick question time over a coffee.
I’m glad Dave is fighting for just some civility for ALL people who happen to be patients
Dave –
Thanks for writing this and you totally nailed it!
I can relate to your article on so many levels and have had similar experiences.
Recently I was contacted by a well known & national Pharmacy via a third party, a Health Media Corp “CEO/Founder,” who shall remain nameless.
He connected with me on LinkedIn and we set up a time to speak – Of course he canceled and rescheduled 15 minutes before we we were set to talk. When we finally did chat, he talked about his “very successful company,” and how he was in charge of his national client’s website, blog and social media presence.
Not so ironically, it was obvious that didn’t he know “jack” re: The Diabetes Online Community or Social Media.
Then he asked me to write a series of articles for his client’s website & blog re: living with diabetes and he seemed shocked when I brought up the subject of payment.
Wasn’t exposure on his client’s website and blog enough?
Nope, not nearly enough.
He can get paid for his time & hard work but I shouldn’t expect to?
As Patient Advocates we bring our knowledge, our skills, our time and our blood, sweat and tears to the table – Damn right we deserve to be compensated!
I love this post.
I have finally been able to negotiate being paid, but the offer is for a full-time position / salary exactly the same as what I first made out of undergrad. It’s the first chance I have had to do patient-centered design of tools for precision medicine, but I want to make sure I am being treated fairly.
I would like to know: how do you determine your fair value? And is it better to accept an offer as an employee or an advisor?
Thanks for posting this, Andrea. When you mentioned this on Facebook I didn’t realize it was about a JOB. That’s a whole different kettle of fish.
My view is what they say about all kinds of sales: for every sale there’s a buyer who thinks it’s worth the price and a seller who thinks it’s worth that too. A major factor is how many other people could do the same for them. Another is whether the price is worth getting out of bed for.
In other words, there’s no single answer. Some people say to get as much as you can out of ’em, with elbows flying, like “cash rugby” or something. I’m more interested in the right mix of value (for each) and sustainability.
Just remember that they don’t hold all the cards (and I assume they’re someone you’d WANT to work for). You have something they want, too.
In your situation I might say “I’d like to do the work, but honestly this is what I was paid right out of college. I was expecting something more like $x. Is that possible? If not, like if there’s some question about the value of my work, how about we try it freelance for six months [or three or whatever], then decide whether we both want to extend it or convert it?”
Of course you’ll need to somehow factor in the value (to you) of whatever benefits they offer. Most companies have a flat percentage that they assume gets added to salary; long long ago at my employer that was 23%. They should be happy to share that number, so that for instance if you were going to be paid $1000 for x hours of work, you’d instead be paid $1230 as a consultant.
In short, be empowered and express yourself, in a spirit of partnershp and finding a mutual solution. Sounds like participatory medicine, eh? :)
Dave, I wrote a similar post around the same time you posted yours. I started as a graphic designer, so I was sadly used to people asking for lots of work for free (claiming: good exposure, fun, quick and easy).
When people try to guilt me into volunteering, I am quick to provide them a long list of the unpaid work I already do, in addition to be very unwell, working a day job, and keeping a home without help.
http://blog.chronicarly.com/should-patients-be-paid/
I love that this post continues to generate dialog 18 months later!
A hefty Facebook discussion broke out yesterday (which triggered Amanda and Carly’s comments above) when John Nosta posted this 2007 three minute video of famed science fiction writer Harlan Ellison delivering A Scathing, Brutally Honest Rant About Not Working for Free. Plenty of cussin’!
To make it easier to share this post, I gave it a memorable shortlink: bit.ly/rattyboxers
This has come up again, years later, in a Facebook post by super-e-patient Janet Freeman-Daily. Amy Morrison Regenstreif added this tale:
“We talked about this when we met …. every time we speak we should be paid… you are way nicer than me ❤️… a cancer group once told me that I should just want to “help people ” with all my knowledge….. I then asked her who else speaking and are they doing it for free….. she said no … I then said do you realize that you are asking a person with continuous cancer for 14 years (at that time) to speak for free? That you are telling me my time and life is worthless? She was speechless and embarrassed and deserved it.”