For two years I’ve blogged about DevDays, the twice-annual software developer conference for the FHIR software standard for health data. November 17-20 was this fall’s edition, and in the opening session, Hannah Wei gave a keynote unlike any other.
Fifteen minute video:
Hannah is a “long COVID” patient – one of the 25-35% of COVID-19 patients who don’t get better. Some stop “being sick” for a while, but relapse; others never really get better. Dr. Anthony Fauci, head of infectious diseases in the US, speaking November 7 with the American Medical Association: “We do know, for absolutely certain, that there is a post-COVID-19 syndrome.”
The really bad news is that as if COVID-19 weren’t enough, medicine doesn’t yet understand Long COVID, a condition that can be dire and incapacitating. So these patients are really in a fix. (More info on this below.)
So, what do they do? They’ve banded together online into several communities and started studying themselves. They’ve defined what features of the condition they want to keep track of, they’ve conducted two surveys so far, and their work has finally started to get the attention of the medical establishment: The BMJ, JAMA, NIH, Dr Fauci, etc.
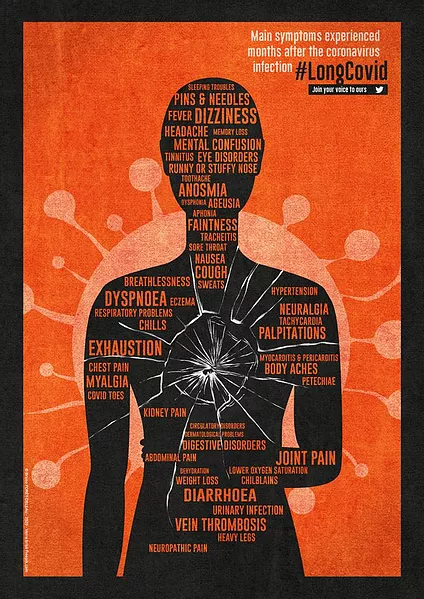
It’s a real medical mystery unfolding in real time, with real human consequences: lives consumed with a bizarre range of symptoms. (The orange graphic here was created by a member of LongCovidSOS, a British patient group.)
Listen to what Hannah says in her speech above, about her own experience and what her patient community wants from the health IT community.
Here are additional links:
CBS 60 Minutes
The Sunday after DevDays, “60 Minutes” had a 13 minute segment. It’s fascinating and a little terrifying. Transcript here.
MIT Technology Review and The Atlantic
Hannah and several of her fellow researchers were the subject of two significant pieces in August. First, in MIT Technology Review, Covid-19 “long haulers” are organizing online to study themselves. The article has good, vivid descriptions of the disease.
A week later the superb science writer Ed Yong penned a piece about them in The Atlantic. The headline alone sums up the importance of the patients’ contribution and urgency of their work:
Cited by the CDC, BMJ, and Francis Collins
The patient researchers’ May survey was accepted into academia by being cited in The BMJ in May in Management of post-acute covid-19 in primary care, and again a few days before DevDays when their reports of symptoms were referenced three times by the Centers for Disease Control and Prevention in their posting Late Sequelae of COVID-19. In September, NIH Director Francis Collins posted about them on his Director’s Blog.
Note: all the above articles arose out of the patient-led survey these people conceived, designed, executed, laboriously analyzed, and reported. Evidently they did a good job! (Collins correctly called them “citizen scientists,” a term that harkens back to the Wired article of the same name in 2001.)
JAMA describing the syndrome
Now we get into assessing the urgency, and starting to weave the patients’ observations into establishment medicine. It doesn’t get more “establishment” than JAMA, the Journal of the American Medical Association. A day after Hannah’s keynote they published A Proposed Framework and Timeline of the Spectrum of Disease Due to SARS-CoV-2 Infection: Illness Beyond Acute Infection and Public Health Implications.
The article underscores the difficulty of understanding what the heck is going on after the “acute” phase – the familiar dry cough / fever / etc. Look at how often it can happen – and it can happen without even being sick enough to be hospitalized:
In one study, 87% of 143 previously hospitalized patients had 1 or more persistent symptoms 60 days after the date of initial COVID-19 symptom onset.
These late sequelae do not appear to be necessarily limited to persons requiring hospitalization.
Here’s how one illustration depicts the state of medical knowledge about it today:
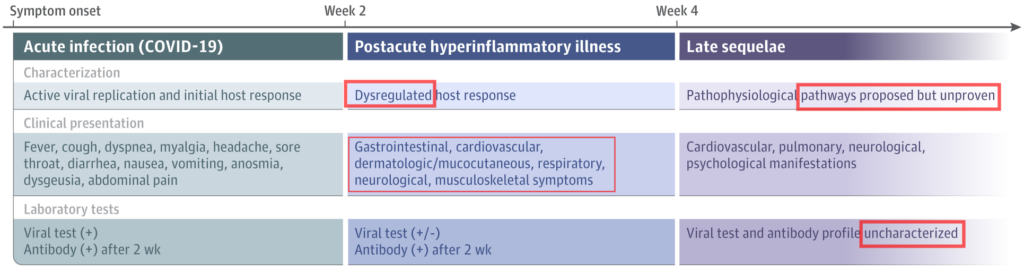
- Left column: acute (traditional symptoms)
- Center: post-acute. Note: “dysregulated” means “out of control.” Yikes. And note in the lower box how different these symptoms are, compared to the acute phase. (What the heck is this thing??)
- Right column: later (long COVID). When science says “pathways unproven” or “profile uncharacterized,” it means “Y’all are on your own – we have no freaking clue yet.”
This is exactly what long COVID patient researchers are working to document, to “characterize” – in their terms, in their experience.
Lancet editorial: Facing up to Long COVID (12/12/20)
Here’s the editorial (it’s open access). Kudos to Lancet for recognizing the importance of basing the work on patient perspectives!
“When the doctor is a long-hauler” (NY Times)
For physicians who may still be skeptical (because they only trust other docs), I give you this, from Shannon Gulliver Caspersen, M.D. in October:
I am a physician who contracted what was initially a fairly mild case of Covid-19 in early March. Seven months later, I remain substantially debilitated, with profound exhaustion and a heart rate that goes into the stratosphere with even the tiniest bits of exertion, such as pouring a bowl of cereal…
Stratospheric heart rate from pouring a bowl of cereal! What is this thing?
Please, docs: as homework, please examine what in your training or your culture taught you not to believe things that didn’t come out of another doc’s mouth. And please remember that all medical care starts with listening to the patient’s subjective symptom report – the “S” in your SOAP notes. And remember Osler’s famous words about listening to the patient.
What does this mean for you and me?
First, for you personally, it’s extra reason to avoid getting this disease. If you’re not motivated by fear of death or hospitalization, remember this additional syndrome that’s totally not understood and strikes (Fauci says) 25-35% of all COVID-19 infections.
On another level, this is a classic example of e-patient communities: empowered, engaged, and enabled by the internet, they’re banding together to go beyond what medicine can offer yet.
“Long haul”? “Long COVID”? PAC? The debate on what to call it
Now that establishment healthcare (the thing that denied it, early on) has gotten its mitts on it, they seem to want to put their own name on it, and are debating what to call it.
- The BMJ Blog, Oct 1: a group of patients authored Why we need to keep using the patient made term “Long Covid”
- VeryWell Health, 11/8/21: Experts Say COVID-19 ‘Long-Haulers’ Need a New Name, including Fauci’s focus on what doctors need … and an insurance-oriented guy saying “an official name is also important because it’s actually one of the first steps before we can create billing codes.” Of course in the US it’s all about the billing codes.
My view: calling it “post” anything installs an assumption that it’s NOT a continuous condition – an assumption that could be hard to undo once we eventually figure out what this thing is.
I mean, the initial error was to assert that the disease was over after XYZ occurred. To now call the later symptoms “post” would be to enshrine the assumption that it was ever over! All we really know today is that it’s the long version of COVID-19.
It would also be a great precedent to honor the people who first identified and cataloged the symptoms, in the same way that many diseases are named for the person who first described them: Parkinson’s, Raynaud’s, Cushing’s, and many many more.
Have another look at the title of Ed Yong’s August article:
Long-Haulers Are Redefining COVID-19
Without understanding the lingering illness that some patients experience, we can’t understand the pandemic.
See what I mean? Let patients help. Listen to patients. Welcome their contributions. Collaborate with them, in the style of participatory medicine.


Really interesting and foreboding. Thanks so much for this.