I want to download all my data from my 14 years as a patient at Beth Israel Deaconess Medical Center. What button should I push?
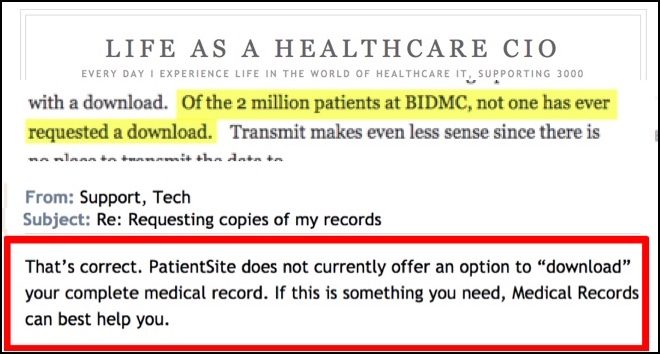
In June you said on your blog (left, top) and on MedCity News that no patient has ever asked for that, but your tech support says you don’t have a way to do it (see red outline).
Tech Support said I should call Medical Records. I did, and they said they can’t deliver things electronically. So where is the link you say nobody has ever used?
As you recently told MedCity News, we’ve been friends for years. Through your blog I’ve long known the excellence of your BMI, your kayaking skills (including rescues), your knowledge of mushrooms, your Unity Farm; in return, all I’ve been able to teach you is how to use Uber when we visited London together in April, on Bob Wachter’s team advising the NHS England. You are a remarkable human being in many ways.
 But professionally, you’re driving me crazy. After I tried to help someone download all my data, I created this GIF. People on Facebook thought it was funny.
But professionally, you’re driving me crazy. After I tried to help someone download all my data, I created this GIF. People on Facebook thought it was funny.
Stop saying patients don’t want this. ENABLE it.
It feels like you keep dissing patients who want to be actively involved in their care, and it feels like you’re actively standing in the way of data sharing. Look how you started that June post above, re VDT (“patients must be able to View/Download/Transmit their data”). As I said in my MedCity ENGAGE speech last month, you slander activated patients:
- “Viewing is great – we’ve done that at BIDMC since 1999 for all patients and all data.”
- Um, no. There’s lots of information in your computers I still can’t see (e.g. my 2007 in-patient records), and until OpenNotes I couldn’t even view my visit notes. Do you not consider those part of “all my data”? I do.
- “Download makes little sense since at the moment there is nothing a patient can do with a download.”
- As I said in that speech, this is a “chicken-and-egg error”: instead of kindling this, to create the new ecosystem we want, you stand motionless and say “See? Nothing’s happening.” There are numerous companies who want to absorb your data (see below), but you offer no way to do it. Don’t blame them for that!
- It’s exactly the argument we used in the typesetting industry 30 years ago when desktop publishing was starting to eat our lunch. You know what we learned? We learned that to innovators, data is fuel. I even said that in a 2010 speech (video) to AHRQ’s IT grantees and contractors.
- Lesson: It’s perverse to starve innovators and then say they haven’t produced anything. Perverse. In desktop publishing, when consumers got their hands on the data and could share it with innovators, then innovation went wildfire. That’s what we want in healthcare. Don’t say there’s no point starting because nobody’s started.
- “Of the 2 million patients at BIDMC, not one has ever requested a download.”
- I don’t have access to Putin or Wikileaks so I can’t know what’s in your emails, but: see the screen captures above. How can you say this with a straight face? Do you know you don’t offer a way to request a download?
- Again, I’ll say it’s perverse to not offer something and then broadcast that nobody has used it. Stop dissing my people!
- “Transmit makes even less sense since there is no place to transmit the data to.”
- Another chicken-and-egg violation, just like #2 above. Those companies I mention want to offer transmit, too. But they can’t develop it because you’re not sending it!
- Several of them have come to me asking for help in figuring out how to get my data out of PatientSite. Epic, Cerner and others are more cooperative than you, John; would you like me to connect you with them?
- I recorded a screenshare demo for them, walking through every bit of PatientSite … I told them I don’t mind if they see my intimate details, because I’m a health data nudist: I don’t care who sees what, if it helps the cause of patient power. As they watched, they kept shaking their heads at the hurdles everywhere, and it kinda made my head spin, too – the first time I walked someone through it, I created that GIF above. (I can share the walkthrough video if you’d like.)
 Know what we want, John? We want a health data spigot: hook up the pipes and let ‘er flow! That’s why this is my profile picture on Twitter and Facebook and it’s on the GetMyHealthData site. (Click it.) Can you do that for us?
Know what we want, John? We want a health data spigot: hook up the pipes and let ‘er flow! That’s why this is my profile picture on Twitter and Facebook and it’s on the GetMyHealthData site. (Click it.) Can you do that for us?
This isn’t the first time we’ve been through this.
Back in 2009 we both ended up on the front page of the Globe after you said in 2008 you had an interface for us patients to send our data to Google Health. When I tried to use it, we discovered that you didn’t send Google my medical record, you sent my insurance billing history, which was full of madness: it said I had an aortic aneurysm, metastases to the brain, non-rheumatoid bitricuspid valve disease, and more.
All that garbage is in my insurance billing historybecause of various common billing practices that insiders tell me are either questionable or outright corrupt: upcoding, billing codes with no evidence (e.g. “bone & cartilage disease” when my tongue metastasis was examined), and perhaps some outright fraud (e.g. that valve disease dx on a visit to treat my femur metastasis(?!?)). I imagine a CIO can’t fix that, but you certainly could have known “This data is crap – we can’t send that to Google!”
(Have you read Wachter’s book The Digital Doctor? It has a great term for claims data: “this waste product of administrative functions.”)
It’s ironic that Google Health took the hit for it and they’re the ones who ultimately shut down from the bad publicity. They were even blamed on the Information Quality Trainwrecks blog, when the problem was the data you sent them.
What really gripes me is that when this hit the newspapers (4/13/2009), you blamed it on patient naïveté: as I’m sure you remember, after our concall your first draft of a response said “We now understand that claims data can be confusing to patients.” When I read that to my wife, she said “That’s insulting! The data they sent Google isn’t confusing, it’s wrong!”
Let patients help create the future, John.
Your words in that June post are a little bit like saying in 1994, “Who needs a web browser?? Nobody has ever tried to access a web page.”
Help create the future, John. Or at least stop saying nobody wants it. Give me a health data spigot, to actually get all my data out. For all patients, all data – “like it’s 1999.” We’ll quickly demonstrate who wants what.
==========
Rest of this short series: (added 5/31/17)
- November 9: He replied in a post mysteriously titled What is patient and family engagement? – “mysteriously” because instead of answering its own question, the post puts up an almost Trump-like diversionary wall, changing the subject.
- November 22 : I replied in Dear John: I still want to download my records! Gimme My DaM Data!, saying also that I was finished with asking nicely; “I’m ready to call it non-negotiable demands.”
- November 28: I added a 15 minute screen-share video, walking through what I can see in my portal: How PatientSite handles interop (not). A data nudist walks through his chart. (I created this to show app developers how to screen-scrape the data from PatientSite that is NOT AVAILABLE FOR DOWNLOAD.)
That was the end of that: he hasn’t replied since. I’d love to continue the conversation. But for it to start honestly, you have to retract your assertion (see screen capture at top) that no patient has ever tried to use that button(“Of the 2 million patients at BIDMC, not one has ever requested a download”) that you don’t offer.


Why not make BIDMC the first institution to support the HEART protocols for patient-directed health record sharing?
Yes, I have experienced the same game, different players, multiple countries. My husband also, I heard him explain patiently that the HIPAA regulations were not put in practice to deny him access.
Another individual was told they could not have their mental health records delivered to them only to a licensed psychologist. The person explained they were a psychologist but no the answer was not for treatment they paid for.
Parents of a child in Florida were told they could not have copies of the chest xray of their child because their billing was not verified, even though they paid cash for the xrays and reading. The child went into respiratory distress in the delay between madness and getting the records.
When another individual requested records they were 2 dollars a page and they could not choose the information they wanted. The lawyer got the information and curated for no payment.
Please be a pioneer at Beth Israel and an example, stop the madness and work with patients for open informed health information that they have already paid for.
No surprise Amy that “”Another individual was told they could not have their mental health records delivered to them only to a licensed psychologist. The person explained they were a psychologist but no the answer was not for treatment they paid for.” I had to intervene for an exactly similar event here.
Although most legislations in Europe allow patients to get a copy of their medical record there are always hospitals and physicians who refuse to do what law/regulations prescribe. Then, it takes a determined and well informed patient to get what he has the right to ask for, more or less the patient kind similar to e-Patient Dave. The question is how many patients can endure to fight with health systems…
My health system (to remain nameless in Northern California) does not have OpenNotes, and I can’t view (or download) important documents related to my condition. Why is it important for me to have access to this information?
Two reasons:
1: People in healthcare wish more patients were participating in research, but my own health system is blocking me from downloading the files I need in order to participate in said research.
2. If I were looking for clinical trials I would need these documents. How can I be active in my care if I have to jump through hurdles to get this stuff?
Pardon me for shouting, but: Liz is reporting that NOT HAVING ACCESS TO HER RECORDS IS IMPEDING HER ABILITY TO PARTICIPATE IN CLINICAL TRIALS AND ACCELERATE RESEARCH.
Why not publish the walkthrough for all to see?
Yes, I will.
Just to complete this thread, I did publish that walkthrough three weeks later, as noted in an addition to the end of the post. https://www.epatientdave.com/2016/11/28/vid-how-patientsite-handles-interop-not-a-data-nudist-walks-through-his-chart/
A lot of comments and shares are coming in on the Facebook post of this.
From Facebook – Dale Hammerschmidt MD, retired, U of Minn school of medicine:
Since I’ve now been retired for two years, I don’t know about recent progress. But I was struck by how poor the planning had been for information to get to patients from our medical record when we went to an extramural EMR vendor. It was as though the vendor didn’t consider it a priority, and neither did the private hospital outfit that had bought our hospital.
The information is embargoed for about a week, to give the physician the chance to contact the patient directly or to deal with other special concerns (that’s very nice, but sometimes dangerous — as when I was peeing blood and needed to know my anticoagulation status — it took ten days to find out). The lab results are then presented in an ASCII convention for rendering scientific notation, which nobody understands, and with “normal” ranges that are seldom physiologic (as opposed to statistical).
If you need a bunch of things from the record because you are seeking consultation or changing providers, you basically have to order a paper print-out (for which there is usually a long back-up). There are no links to explanatory materials (that, of course, is an unfunded mandate that falls on the physicians — the hospital scares the hell out of the patient with uninterpretable gibberish, and it is the doc’s job to fix it).
For the most common problems for our hematologic oncology patients, we had explanatory handouts — but then the hospital “risk management” people saw that as a risk-related activity over which they had no control, and they insisted we stop. The materials they substituted were not worth a cold hunk of [several expletives deleted], and patients commonly found them insultingly juvenile.
So (a) we’re still a long way from doing this well, largely because it is not revenue generating, and (b) nobody should be surprised that I retired ;-).
When I asked Dale for permission to cross-post this here, he said: “Sure. If you need specific examples for a longer piece at some time, I can probably oblige you. What I almost added was that the difficulty getting records OFTEN meant that I saw extramural consultations with NO advance information whatsoever. A huge waste of time and an inconvenient delay, sometimes a dangerous one.”
LOOK: THIS SENIOR PHYSICIAN REPORTS THAT NOT HAVING THE RECORDS IS A HUGE WASTE OF TIME AND SOMETIMES DANGEROUS. WHAT IS THE QUESTION ABOUT THE NEED TO DO THIS??
For way to many people, they do not know how hard it is to get complete and accurate records until they need them…and then when they do it is in a time of health crisis. This blog is great.
I am a family physician. I was with my husband at his colonoscopy today. While he was recovering , I started what I realized is a common practice of mine when I have a procedure or when I accompany a family member to the hospital, trying to figure out how to get access to the records. NOT the “labs were normal” type of summary but real records.
When I as the patient request, at the time of registration, for records to be sent when they are available, I have been told (honestly) to come back at least 5 days later, go to “a room in the basement” (medical records) to request a form to sign so that (maybe) records will eventually be mailed. There is no system to have access to records for patients and family members. It takes way too much time and energy.
And as a primary care physician, the same can be said. When I refer a patient somewhere, say to the ER, I hardly ever get records. When I call to ask, I am told I need a form signed and that they will eventually be (again maybe) sent. This is NOT continuity of care. This is wasted time and money for everyone. Tests have to be repeated because we can’t get access.
As a caring family member, a patient advocate and primary care physician, I fully agree with you, Dave.
Thanks, Sharon.
There are still people who deeply disagree that the current situation is a problem that needs to be fixed stat. Could you offer some first-hand examples you’ve seen where better care has been impeded by lack of information that exists in another system but could not be brought to the point of need?
Thank you, Dave, for so clearly calling out this issue.
Just adding to the chain — my blog post from 2012 when Dr. Halamka and Gov. Patrick kicked off the Mass HIway http://www.awesomecancersurvivor.com/2012/10/massachusetts-kicks-off-the-health-information-highway.html Over 4 years old – I have yet to have a doctor share information via the HIWay. I can log in and view/download my records from my primary care and my oncologist – by going to separate portals. No way to combine this information.
I was on the HIT Policy Committee for three years. It was an exasperating experience for me – perhaps it was my rookie status, perhaps it was my impatience with the lack of immediacy. The EHR Incentive Program incentivized the end points but they forget to incentivize the most important piece – communication and sharing!
From CMS: “The Stage 1 final rule set the foundation for the EHR Incentive Programs by establishing requirements for the electronic capture of clinical data, including providing patients with electronic copies of health information.
The Stage 2 final rule expanded upon the Stage 1 criteria with a focus on ensuring that the meaningful use of EHRs supported the aims and priorities of the National Quality Strategy. Stage 2 criteria *encouraged* the use of health IT for continuous quality improvement at the point of care and the exchange of information in the most structured format possible.”
So much money spent building the end points, no money spent on making sure collaboration and sharing can take place.
Too little too late. The Ivory Tower of Healthcare still in full effect.
In 2015 at the ESMO (European oncology) conference I met Bettina Ryll, Ph.D., a research scientist whose husband died of malignant melanoma a few years ago. On this Facebook post she said:
As a cancer survivor (http://bit.ly/a7vkblogen) I agree 200%.
With Andaman7 (http://www.andaman7.com), we are open to work with *any* hospital or EMR vendor to enable the download of their medical data to patients.
Now, we only need a YES from some future minded and patient oriented doctors and hospitals…
Dr Halamka, I also receive care at BIDMC (neurologist, urologist, ophthalmologist, physical therapist). I want to download my complete Medical Record. Now I shlep paper records to Boston Children’s, Partners, and Mt Auburn where I also receive care.
Thanks for the addition, Danny. Every voice counts, every life matters!
It is amazing how quickly a patient becomes knowledgeable about his treatment when he receives his records–not getting them readily is the norm, however. Many cancer patients don’t know or were simply overwhelmed at the time of diagnosis to digest the details, so are at a tremendous disadvantage to discuss their own care with their own doctor.
Having the images and the records can often reveal that a tumor was noted 1-2 years ago while looking for a broken rib, but never followed up with either patient or ordering physician. The first paragraph, “no broken rib”, might be the last phrase the doctor reads. But the patients will read to the last, likely with difficulty, and may well see, “mass seen on…” as an incidental finding!
Until patients receive all their data and in a meaningful way, they are NOT well-cared for by any one provider or any large medical system. Naturally all of this opens the door to complaints about overlooked tumors, treatments that did not match the diagnosis, procedure which were billed for, but not received–but without this kind of patient oversight, we will never have true health reform.