A quick note to draw your attention to two posts this week.
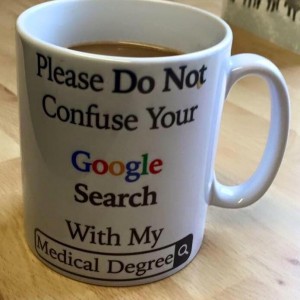
First, the coffee mug at right has gone crazy viral on Facebook, with over 100,000 shares in the first few days. It’s a great big mudpuddle splash, smack into the changing e-patient reality compared to how many doctors were trained. Yes, there’s junk on the internet and some people (including some patients) are loco. That does not mean patients should just shut up and expect the doctor to know everything. So, on the e-patient blog I posted this explanation:
The truth about that “your Googling and my medical degree” mug
Second, yesterday’s Washington Post had a great, well researched and comprehensive piece about medicine listening to patients. Reporter Susan Allard Levingston interviewed and cited many people I know and several I don’t, including my doctor Danny Sands, Mayo’s Victor Montori, ACOR, SmartPatients, Inspire.com, PatientsLikeMe, the BMJ’s patient partnership program that I’m a part of, and more. My post about it:
Washington Post nails it about patient-clinician partnership
The timing of this clash couldn’t have been more perfect to illustrate the topic of my Grand Rounds as Visiting Professor at the Mayo Clinic last March: We are at the cusp of a profound paradigm change in medicine.
The whole concept of what “patient” can be and do is evolving – but most people don’t know it. Many patients and many docs think patients couldn’t possibly know anything useful; that is no longer the case, and culture clash is happening.
Honestly, this is the work of evangelism – spreading the word, making the case. And you know people are starting to notice when “the empire strikes back,” as illustrated by that coffee mug piece.
Please:
If you don’t yet know about the Belgian health department’s anti-googling campaign (taxpayer-funded!), and you don’t yet know about the British teen who died because her docs told her to stop googling, go read that coffee mug piece. Then read the comments from patients who helped their docs make a correct diagnosis. Then skip over to the Washington Post piece, and read about “the real reality.”
And spread the word! Culture change only succeeds when people spread the word. Thank you!


 How perfect: a month to the day after her June 24 bilateral knee replacement, today the physical therapist gave Ginny the thumbs-up to drive.
How perfect: a month to the day after her June 24 bilateral knee replacement, today the physical therapist gave Ginny the thumbs-up to drive. This means she has the strength and mobility to be able to respond safely to traffic situations. That’s a heck of a recovery after having both knees cut open, eh?
This means she has the strength and mobility to be able to respond safely to traffic situations. That’s a heck of a recovery after having both knees cut open, eh?

 #3 in a series. Previous entries:
#3 in a series. Previous entries: